-
A.C.L. Reconstruction (Hamstring Graft)
0 – 2 weeks:
- Weight bearing as tolerated (allowed full weight bearing)
- Take bandages off after 3 days, leaving waterproof dressing in place
- Reduce swelling e.g. tubigrip, ice (covering knee with gladwrap), elevation
- Commence range of movement exercises e.g. heel slides, sustained stretches into
flexion and extension, stationary bike as able
- Co-contractions i.e. isometric gluteals, hamstrings and quadriceps contraction
- Calf raises and hip abduction in standing
- Single-leg balance exercises as able
- Gentle hamstring stretches
- No open chain quadriceps strengthening e.g. straight leg raises, leg extensions
2 – 6 weeks:
- Dressings removed after ~ 10 days, wound checked
- Commence scar massage / desensitization
- Continue to reduce swelling
- Push range of movement exercises, especially extension range and bike, aiming for full range by 4 weeks
- Progress co-contractions into standing
- Commence closed-chain quadriceps strengthening as able, e.g. squats, lunges, step-ups, focussing on inner-range control into extension
- Progress to single-leg calf raises as able
- Hip strengthening in side lying, progressing to stability exercises in standing e.g. step up/down, 4-way hip with elastic
- Commence gentle active hamstrings strengthening, no resistance
- Progress balance exercises, but remain on stable surfaces
6 weeks onward:
- Continue to push lower limb strength and endurance, including resisted hamstring strengthening, hip stabilisation exercises
- Progress balance exercises, e.g. wobbleboard, dura-disc, foot placement drills
- Can commence jogging on minitramp at 6 weeks, treadmill at 8 weeks and straight-line running outdoor at 10 weeks if progressing well
- Can add more advanced proprioception exercises at 12 weeks, e.g. jumping and hopping (emphasising good landing technique), lateral movements
- Can commence low-risk activities, e.g. outdoor cycling, swimming, aerobics classes, bushwalking after 12 weeks
- Add sports specific strength and proprioception exercises after 12 weeks
- No open-chain quadriceps strengthening for 4 months
- Return to sport 9 -12 months
-
Lateral Ligament Reconstruction
0 – 2 weeks:
Non-weight bearing in backslab
Reduce swelling with elevation2 – 4 weeks:
Dressing, backslab and stitches removed
Fitted with CAM boot, weight-bearing as tolerated
Commence scar massage / desensitisation4 – 6 weeks:
Commence eversion range of movement and strengthening
No inversion range of movement6 – 12 weeks:
Remove CAM boot, wearing supportive footwear at all times
Continue evertor strengthening
Commence dorsiflexion / plantarflexion range of movement, not pushing plantarflexion too hard
Commence calf strengthening and proprioception exercises
Wear ankle brace for all walking12 weeks onward:
Can commence inversion range of movement and strengthening
Wear ankle brace for higher risk activities, e.g. walking on uneven / rough surfaces, return to running and sporting activities
Can commence straight line running after 3 months
Return to low-risk sports, e.g. golf, running after 4-5 months
Return to high risk sports, e.g. football codes, cricket, netball, basketball, after 6 months -
Tibialis Posterior Reconstruction
Tibialis Posterior Reconstruction
(FHL Transfer and Calcaneal Osteotomy)0 – 2 weeks:
· Non weight bearing in backslab
· Reduce swelling with elevation2 – 4 weeks:
· Dressing, backslab and stitches removed
· Fitted with CAM boot and varus heel wedge
· Remain non-weight bearing4 – 6 weeks:
· Partial weight bearing in CAM boot with varus heel wedge
· Commence gentle active inversion range of movement, relaxing to neutral6 – 12 weeks:
· Mobilise full weight bearing
· Remove boot after 8 weeks; convert to supportive shoes with orthotics (varus heel cup and medial longitudinal arch support)
· Commence dorsiflexion and plantarflexion range of movement
· Commence calf strengthening with theraband12 weeks onward:
· Commence calf strengthening in standing
· Commence inversion strengthening -
Tendo Achilles Repair Post-operative Protocol
0 – 2 weeks:
- Non-weight bearing, front slab on ankle
- Rest and keep leg elevated wherever possible
- Can perform general, non-weight bearing lower limb strengthening, e.g. straight leg raises, leg extensions, leg curls, hip abduction in side lying etc.
2 – 8 weeks:
- Stitches removed, removable front slab applied
- Remain non-weight bearing
- Remove front slab three times per day and perform active ankle dorsiflexion to less than neutral, then relax back into plantarflexion
- Continue general lower limb strengthening
8 – 10 weeks:
- Commence weight bearing as tolerated with heel lifts in supportive footwear
- Commence physiotherapy, focussing on passive and active range of movement
- No resistance training for calf at this stage
- Perform scar massage / desensitization
10 – 12 weeks:
- Gradually remove heel lifts in shoes
- Commence calf stretches in standing
- Commence theraband strengthening of calf
12 weeks onward:
- Can commence calf raises from the floor, starting on both feet and slowly increasing weight through operated side as comfort allows
- Can progress calf strengthening to a step when able to perform 15 single-leg repetitions on the operated leg
- Aim for dorsiflexion > 8 cm (toe from wall test)
- Can commence jogging when able to perform 15 single-leg calf raises off the step (normally 6 months post op.)
- After 6 months can introduce eccentric calf strengthening program to encourage tendon remodelling and increase strength.
-
Non Operative Treatment of Tendo Achilles Rupture
First 10 days after rupture:
- Patient in equinus front slab mobilising touch weight bearing.
- Equinus front slab to remain on at all times.
- Keep leg elevated.
10 days to 4 weeks:
- Patient in removable equinus front slab.
- Mobilise touch weight bear.
- Remove front slab for 5 minutes every hour whilst sitting with the injured leg hanging and perform active ankle dorsiflexion followed by passive plantar flexion. Ankle not to be dorsi-flexed beyond neutral during the active dorsiflexion component of the exercises.
4-6 weeks:
- Patient in walking boot with heel raise.
- Continue with active dorsiflexion and passive plantar flexion exercises (as previously described).
- Continue to mobilise touch weight bear wearing the walking boot day and night except for period when performing exercises.
6-8 weeks:
- Patient to weight bear as tolerated in walking boot with heel raise.
- Continue exercises as previously described.
- Patient allowed to remove walking boot at night.
8-10 weeks:
- Remove walking boot and mobilise weight bear as tolerated in supportive shoes.
- 1 cm heel raise in shoe.
- Commence physiotherapy, focussing on active and passive range of motion.
- No resistance training for calf at this stage.
10-12 weeks:
- Gradually remove heel lift in shoe.
- Commence calf stretches in standing.
- Commence theraband stretching of calf.
12 weeks onward:
- Can commence calf raises from floor, starting on both feet and slowly increasing weight through operated side as comfort allows.
- Can progress calf strengthening to a step when able to perform 15 single-leg repetitions on affected leg.
- Aim for dorsiflexion > 8cm (toe from wall test).
- Can commence jogging when able to perform 15 single-leg calf raises off a step (normally 6 months post-op).
- After 6 months can introduce eccentric calf strengthening program to encourage tendon remodelling and increase strength.
Patient Instructions after Knee Arthroscopy
-
Post Operative Instructions
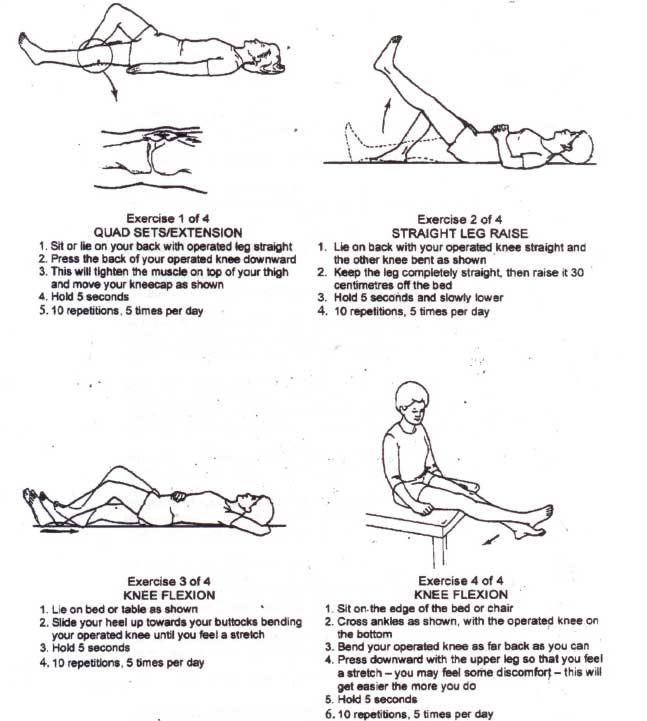
- Immediately post operatively you must commence straight leg raises (SLR) as shown to you by the nursing staff
- Once you can SLR you may get out of bed and walk around, aided by the nursing staff
- You will be discharged the evening of surgery
- If crutches are necessary, the day surgery ward staff will organise
- You may walk normally, using crutches or a stick if needed
- A post-operative appointment should be made for you to see Dr Limbers in his rooms
- Continue your quadriceps (10 SLR exercises helf for 10 seconds, 10 times a day)
- The outer dressing can be removed on approximately 2 days. It can be removed leaving the adhesive dressing on the skin. Apply brown Tubigrip over this. Try not to get this dressing wet
- Take Panadol for pain – 2 every 6 hours if needed
- If there are any problems please contact Dr Limbers rooms on telephone no. (02) 4393 3820 or contact the orthopaedic nursing staff at the hospital
Foot and Ankle
-
Plantar Faciitis Exercises
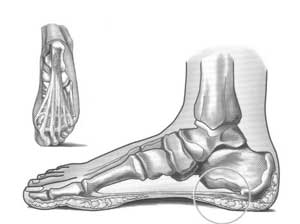 The plantar fascia is a thick band of tissue that arises from the front of the heel bone and fans out to cover the sole of the foot. This band provides support for the arch of the foot and assists with shock absorption when walking and running. Plantar Fasciitis is an overuse condition and more accurately should be described as a degeneration of the tissue, making it very difficult to treat. Risk factors include flat or high-arch feet, reduced ankle dorsiflexion (knee over toes), overweight, inappropriate or non-supportive footwear and tight hamstring and calf muscles.
The plantar fascia is a thick band of tissue that arises from the front of the heel bone and fans out to cover the sole of the foot. This band provides support for the arch of the foot and assists with shock absorption when walking and running. Plantar Fasciitis is an overuse condition and more accurately should be described as a degeneration of the tissue, making it very difficult to treat. Risk factors include flat or high-arch feet, reduced ankle dorsiflexion (knee over toes), overweight, inappropriate or non-supportive footwear and tight hamstring and calf muscles.People with Plantar Fasciitis often report pain on the inside of the heel, which is worse first thing in the morning or after a period of rest. While x-ray may reveal a heel spur (not usually related to pain) and ultrasound may confirm the condition, often a diagnosis is made within the clinic.
Treatment for this condition may include activity modification, orthotics, golf-ball massage, stretches (hamstring, calf and plantar fascia), ice after activity, taping, silicone heel pads, night splints, footwear changes and anti-inflammatories (shortterm relief). Surgery is very rarely indicated.
Plantar Fascia Stretch:
Toes up box, slide foot to floor and push knee forward over toes. Hold 30 seconds, 5 times.
Calf Stretch:
Back leg straight, heel on ground, lunge forward until you feel a gentle stretch in your calf. Hold 30 seconds, 5 times.
Hamstring Stretch:
Belt around foot, knee slightly bent. Pull leg back until you feel gentle stretch behind thigh. Hold 30 seconds, 5 times.
